Abstract
Rationale: Lower airway disease is common in pediatric sickle cell disease (SCD) and is often diagnosed as asthma. This condition may be a risk factor for acute chest syndrome (ACS) and pain episodes. There are conflicting data about whether SCD-associated lower airway disease is due to allergic inflammation, as is typical in non-SCD childhood asthma. However, transgenic SCD mouse models have suggested a propensity toward allergic inflammation, and a recent study in children with SCD suggested allergic sensitization was associated with increased risk of acute chest syndrome (ACS). Allergic sensitization may be a risk factor for pulmonary inflammation and may trigger pain episodes. We hypothesized that allergic sensitization to a panel of indoor allergens would be associated with more frequent ED visits and hospitalizations for pain, ACS, and asthma symptoms in children and adolescents with SCD.
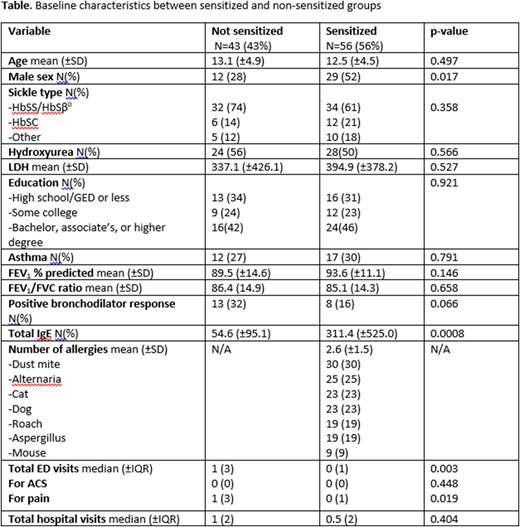
Methods: Patients were recruited from two large academic children's hospitals. Ninety-nine participants with SCD ages 5-21 who were not receiving chronic exchange transfusions completed pre- and post-bronchodilator spirometry and allergy testing at a baseline visit. Allergen-specific IgE in blood was measured to Alternaria, Aspergillus, cat, cockroach, dog, dust mite (D. farinae), and mouse urine protein; we examined baseline characteristics by stratified groups (not sensitized vs. sensitized to one or more allergens) via t-tests, chi square, and Mann-Whitney U tests; we created a count variable with number of sensitizations. ED visits and hospitalizations were reviewed retrospectively two years prior to study entry. Asthma was defined as physician diagnosis in medical records plus at least one home asthma medication (albuterol or controller/preventative medication). We used negative binomial models to examine relationships between atopy [number of positive specific IgE (³0.35kU/L)] and the number of ED visits and hospitalizations, adjusting for age, sex, hydroxyurea use, and head of household (HOH) education level. FEV1 and positive bronchodilator response (³10%) were compared via multiple linear regression and multiple logistic regression.
Results: Participants were 41% male, 66% HbSS or HbSb0 genotype, 52% on hydroxyurea, and 32% had a HOH with a high school education or less [Table]. Twenty-eight percent had a physician diagnosis of asthma, and 57% (N=56) were sensitized to at least one allergen. Allergic sensitization was associated with decreased risk of total ED visits1 (IRR 0.80[0.66-0.97] p=0.022), ED visits for pain (IRR 0.80[0.67-0.97] p=0.019), and fever (IRR 0.63[0.45-0.88] p=0.007), but not associated with a significant difference in ED visits for asthma or ACS. Allergic sensitization was neither associated with differences in rates of hospitalization (total, or for pain, fever, ACS, or asthma) nor with differences in FEV1 percent predicted, FEV1/FVC ratio, or positive bronchodilator response.
Conclusions: In a population of children with SCD, allergic sensitization was associated with decreased risk of ED visits (total, for pain, and for fever). The mechanism for an association between atopy and a less severe phenotype of SCD is unclear. These findings point to potential differences in immunologic endotype/phenotype and add support to the hypothesis that lower airway disease in children with SCD has a different mechanism than typical childhood atopic asthma. Further investigation into the immunologic phenotypes and mechanisms of lower airway disease in children with SCD is warranted.
1All IRR presented are per allergen, adjusted for age, sex, hydroxyurea use, and HOH education level; 95% confidence interval.
Strouse:Global Blood Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.